Trigeminal Neuralgia Diagnosis
Trigeminal Neuralgia –
Do I have it?
Do I have it?
Do you have pain on one side of your face that feels like an “electrical shock” or a “sharp stab”?
Do you think the pain has something to do with your teeth, but your dentist tells you that your teeth are “fine”?
Does the facial pain hit you quickly and last for seconds?
Do certain basic things trigger your pain like talking, eating, washing your face or brushing your teeth?
If you said “YES” to a few of these questions, then you might have classic type I trigeminal neuralgia.
People use many different words to describe the types of pain that can affect one side of the face. When they use words like “electric shock” or “sharp” or “stabbing”, then the diagnosis of trigeminal neuralgia needs to be considered. The next questions that people ask include, “what is causing this pain and what do I do to get pain relief as soon as possible”? These are all great questions, so let’s start with why…
Facial pain – What causes trigeminal neuralgia pain?
Trigeminal neuralgia is also called “tic douloureux”. This was the French name given to one-sided facial pain by Nicholas André in 1756 when he noticed that facial pain patients would contract one side of the face every time they had a severe pain episode. Since then, we have learned a lot about how we feel pain in our face and why some people might develop trigeminal neuralgia in their life times.
The Trigeminal Nerve – Just think of a Tree with 3 big branches
To begin to understand facial pain, you need to understand that we have 2 trigeminal nerves (1 of 12 pairs of cranial nerves); one trigeminal nerve feels the right side of the face and one feels the left side of the face. The trigeminal nerves are like trees in that they have a “trunk” and three larger “branches”. Each branch feels a part of the face (these divisions are called V1, V2 and V3).
Inside the nerve are hundreds of nerve fibers. You can think of each tiny nerve fiber as a “wire” that carries information from the face to the brain to tell us what is happening with our skin, eyes, teeth, etc… Each small sensory wire carries a different kind of sensation back from the face to the brain. For example, there is a set of wires that feel hot and cold, and another set of wires that feel sharp pin-pricks and yet another wire that feels pressure on our teeth.
These wires are all bundled together like the coaxial cable in your home. Like most electrical wires, they are surrounded by insulation called myelin. The myelin insulation keeps the sensory information about temperature, pressure and pain flowing quickly to the brain while preventing the wires from “shorting out” on each other by mistake (when everything is working correctly).
Inside the nerve are hundreds of nerve fibers. You can think of each tiny nerve fiber as a “wire” that carries information from the face to the brain to tell us what is happening with our skin, eyes, teeth, etc… Each small sensory wire carries a different kind of sensation back from the face to the brain. For example, there is a set of wires that feel hot and cold, and another set of wires that feel sharp pin-pricks and yet another wire that feels pressure on our teeth.
These wires are all bundled together like the coaxial cable in your home. Like most electrical wires, they are surrounded by insulation called myelin. The myelin insulation keeps the sensory information about temperature, pressure and pain flowing quickly to the brain while preventing the wires from “shorting out” on each other by mistake (when everything is working correctly).
Facial Pain – When the System Goes “Haywire”
When someone experiences “electrical shocks”, “stabbing pain” and “sharp pain” that come in short bursts (1-3 seconds) and are triggered by eating, talking, chewing, or touching their face, trigeminal neuralgia is likely.
This type of facial pain is consistent with a “neuralgia”. We believe that the tiny wires inside the trigeminal nerve “tree” are starting to “short out” on each other. When a wire that feels cold water on your face shorts out on a wire that is meant to feel sharp pain, the cold water makes the pain wire fire by mistake. This is called “ephaptic transmission”. We believe that this happens when the insulation between these two very different sensory wires breaks down in small spots.
The breakdown of the insulation is often the result of a blood vessel, beating on and heating up the trigeminal nerve at the level of the “trunk” of the nerve. This situation is called “neurovascular conflict” and is often found in patients with type I (classic) trigeminal neuralgia symptoms. The breakdown of the myelin insulation can also be seen in patients with multiple sclerosis (MS).
MS is a condition where myelin insulation tends to breakdown in specific locations and in this case, the myelin breaks down along the trigeminal nerve pathway. As time progresses, the breakdown of insulation can become more severe and episodes of pain that used to be short and rare can become more frequent and intense. Some patients can progress to type II (atypical) trigeminal neuralgia as their condition goes further along.
Facial Pain – When the System Goes “Haywire”
When someone experiences “electrical shocks”, “stabbing pain” and “sharp pain” that come in short bursts (1-3 seconds) and are triggered by eating, talking, chewing, or touching their face, trigeminal neuralgia is likely.
This type of facial pain is consistent with a “neuralgia”. We believe that the tiny wires inside the trigeminal nerve “tree” are starting to “short out” on each other. When a wire that feels cold water on your face shorts out on a wire that is meant to feel sharp pain, the cold water makes the pain wire fire by mistake. This is called “ephaptic transmission”. We believe that this happens when the insulation between these two very different sensory wires breaks down in small spots.
The breakdown of the insulation is often the result of a blood vessel, beating on and heating up the trigeminal nerve at the level of the “trunk” of the nerve. This situation is called “neurovascular conflict” and is often found in patients with type I (classic) trigeminal neuralgia symptoms. The breakdown of the myelin insulation can also be seen in patients with multiple sclerosis (MS).
MS is a condition where myelin insulation tends to breakdown in specific locations and in this case, the myelin breaks down along the trigeminal nerve pathway. As time progresses, the breakdown of insulation can become more severe and episodes of pain that used to be short and rare can become more frequent and intense. Some patients can progress to type II (atypical) trigeminal neuralgia as their condition goes further along.
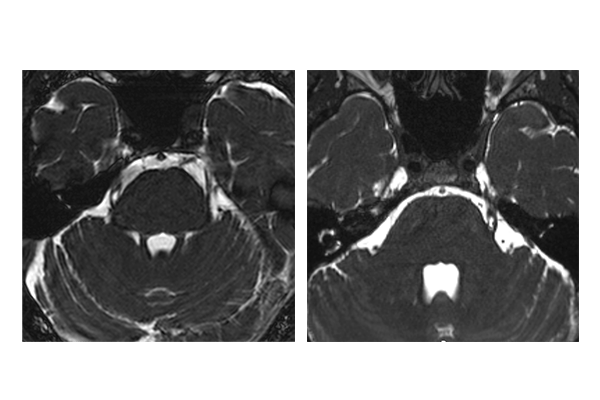
Should I get an MRI scan if I have trigeminal neuralgia?
If you have been diagnosed with trigeminal neuralgia, a magnetic resonance image (MRI) scan is a good idea. The best brain MRI sequences to get include a very high-resolution study often called a “FIESTA” sequence (or a thin-cut T2 sequence) and a post-contrast (T1) study.
The FIESTA study will show an expert whether or not there is an offending blood vessel beating on the trigeminal nerve “trunk” on the same side as your pain. Again, this MRI finding will often be called “neurovascular conflict” and if found on the same side as your pain, is a very helpful datapoint. The post-contrast MRI scan is a good scan to get because this study will rule out other potential causes for facial pain like active multiple sclerosis, tumors and even some vascular malformations (like an arteriovenous malformation).
A word of caution about the MRI
A word of caution about the MRI – An MRI does not prove that you have trigeminal neuralgia.
Only the complete medical picture can suggest trigeminal neuralgia. Also, finding “neurovascular conflict” on the FIESTA MRI study does not necessarily mean that the blood vessel is the cause of your pain. Your entire medical history, physical examination, review of systems, etc. MUST be taken into consideration. That said, a quality MRI tends to be very low-risk and is often worth getting to help your expert team manage treat trigeminal neuralgia effectively for you.
Treatment Options for Trigeminal Neuralgia
There are a variety of treatment options for trigeminal neuralgia and facial pain. All of them start by making the right diagnosis first! Once the diagnosis of trigeminal neuralgia has been made by an experienced expert, treatment options most commonly include:
Medications (such as Trileptal, Tegretol, Gabapentin, Baclofen, etc)
Gamma Knife Radiosurgery (aka, Stereotactic Radiosurgery)
Percutaneous Rhizotomy (using either a balloon, heat or glycerol)
Pain Stimulators
Always consult your expert team before pursuing trigeminal neuralgia treatment. Be certain to ask about risks, benefits, and potential side effects of any treatment you are considering.
Treatment Options for Trigeminal Neuralgia
There are a variety of treatment options for trigeminal neuralgia and facial pain. All of them start by making the right diagnosis first! Once the diagnosis of trigeminal neuralgia has been made by an experienced expert, treatment options most commonly include:
- Medications (such as Trileptal, Tegretol, Gabapentin, Baclofen, etc)
- Gamma Knife Radiosurgery (aka, Stereotactic Radiosurgery)
Percutaneous Rhizotomy (using either a balloon, heat or glycerol)
- Pain Stimulators
Always consult your expert team before pursuing trigeminal neuralgia treatment. Be certain to ask about risks, benefits, and potential side effects of any treatment you are considering.